FREQUENTLY ASKED QUESTIONS
- FREQUENTLY ASKED QUESTIONS
FASHIONABLY HEALTHY EMPOWERMENT SERIES
Amyloidosis is a rare group of diseases characterized by the abnormal buildup of a protein called amyloid in organs and tissues throughout the body. This protein can interfere with normal function and cause damage to affected areas, leading to potentially serious health complications.
Types of Amyloidosis
- AL Amyloidosis (Light Chain Amyloidosis)
- The most common form, caused by the overproduction of abnormal light chain proteins by plasma cells in the bone marrow.
- Affects organs such as the heart, kidneys, liver, and nerves.
- ATTR Amyloidosis (Transthyretin Amyloidosis)
- Caused by mutations in the transthyretin (TTR) gene or by age-related changes to the protein.
- Subtypes:
- Hereditary ATTR Amyloidosis: A genetic condition affecting the nerves and heart.
- Wild-Type ATTR Amyloidosis: Typically affects older adults, primarily impacting the heart.
- AA Amyloidosis
- Results from chronic inflammatory or infectious diseases, such as rheumatoid arthritis or tuberculosis.
- Often affects the kidneys.
- Localized Amyloidosis
- Amyloid deposits occur in a single area of the body, such as the skin or bladder, rather than throughout the body.
- Other Rare Types
- Includes forms like Beta-2 Microglobulin Amyloidosis, often associated with dialysis.
Symptoms
Symptoms depend on the organs affected and may include:
- Fatigue or weakness.
- Shortness of breath.
- Swelling in the ankles or legs.
- Unintended weight loss.
- Tingling or numbness in the hands or feet.
- Enlarged tongue or difficulty swallowing (in some cases).
- Irregular heartbeat or heart failure (if the heart is affected).
- Kidney failure or protein in the urine.
Diagnosis
- Blood and Urine Tests: Detect abnormal proteins.
- Biopsy: A tissue sample confirms amyloid deposits.
- Imaging Tests: Evaluate organ damage (e.g., echocardiogram, MRI).
- Genetic Testing: Identifies hereditary forms of amyloidosis.
Treatment
Treatment focuses on managing symptoms, slowing disease progression, and addressing the underlying cause:
- Medications: Target amyloid deposits or reduce protein production (e.g., tafamidis for ATTR amyloidosis, chemotherapy for AL amyloidosis).
- Organ Transplants: For severe cases affecting organs like the heart or liver.
- Supportive Care: Treats complications such as heart failure or kidney issues.
Relevance to the Black Community
- Awareness and Access to Care: Like many rare diseases, amyloidosis may go underdiagnosed in underserved communities due to lack of awareness or healthcare access.
- Genetic Predispositions: Some hereditary forms, like ATTR amyloidosis, may disproportionately affect individuals of African descent.
Early detection and a multidisciplinary approach to treatment are essential to managing amyloidosis effectively. Collaboration with specialists and access to resources can improve outcomes and quality of life for those affected
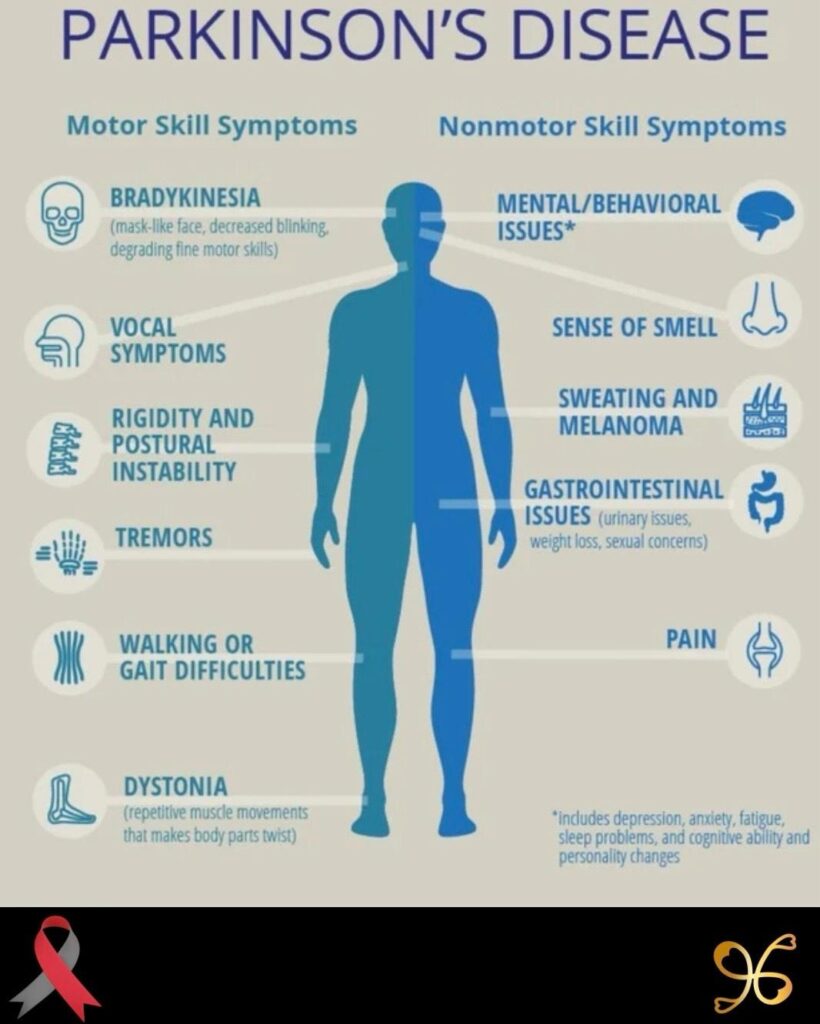
Parkinson’s Disease is a progressive neurological disorder that affects movement, coordination, and various non-motor functions. It results from the loss of dopamine-producing neurons in a region of the brain called the substantia nigra, leading to the characteristic symptoms of the disease.
Symptoms
Parkinson’s Disease has a wide range of motor and non-motor symptoms:
Motor Symptoms
- Tremors: Shaking, typically starting in the hands or fingers, even at rest.
- Bradykinesia: Slowness of movement, making simple tasks time-consuming.
- Rigidity: Stiff muscles that may cause pain or limit range of motion.
- Postural Instability: Problems with balance and coordination, leading to a higher risk of falls.
Non-Motor Symptoms
- Cognitive changes, including memory issues or difficulty concentrating.
- Depression and anxiety.
- Sleep disturbances, such as insomnia or REM sleep behavior disorder.
- Fatigue.
- Constipation and other gastrointestinal issues.
- Loss of sense of smell (anosmia).
Causes
The exact cause of Parkinson’s is unknown, but several factors contribute to its development:
- Genetics: Mutations in certain genes (e.g., LRRK2, PARK7) can increase risk, though hereditary cases are rare.
- Environmental Factors: Exposure to toxins such as pesticides or heavy metals.
- Age: Risk increases significantly with age, typically affecting people over 60.
- Gender: Men are slightly more likely to develop Parkinson’s than women.
Diagnosis
Parkinson’s is diagnosed clinically, as no definitive lab test exists:
- Neurological Exam: Focused on motor function and reflexes.
- Imaging Tests: MRI or PET scans rule out other conditions.
- Response to Medication: Improvement with dopamine-replacement therapy supports diagnosis.
Treatment
While there is no cure, treatment focuses on managing symptoms and improving quality of life:
- Medications:
- Levodopa: Converts to dopamine in the brain to alleviate motor symptoms.
- Dopamine Agonists: Mimic dopamine’s effects.
- MAO-B Inhibitors: Slow the breakdown of dopamine.
- Surgical Options:
- Deep Brain Stimulation (DBS): Implants electrodes in the brain to regulate abnormal activity.
- Lifestyle and Supportive Therapies:
- Physical, occupational, and speech therapy.
- Regular exercise to improve mobility and balance.
- Dietary adjustments to manage constipation and maintain energy levels.
- Mental Health Support:
- Counseling for anxiety or depression.
- Support groups for patients and families.
Parkinson’s in the Black Community
- Underdiagnosis and Delayed Treatment: Parkinson’s may be underrecognized in Black patients due to healthcare disparities or biases.
- Awareness and Access: Outreach and education are critical for improving early diagnosis and care in underserved communities.
- Research Gaps: Increased representation in clinical studies is needed to understand disease progression and outcomes in Black populations.
Living with Parkinson’s
Parkinson’s requires a multidisciplinary approach, involving neurologists, therapists, and caregivers. With proper management, many patients maintain independence and lead fulfilling lives for many years after diagnosis. Early intervention and a supportive network are key to improving quality of life.
Amyloidosis is a rare group of diseases characterized by the abnormal buildup of a protein called amyloid in organs and tissues throughout the body. This protein can interfere with normal function and cause damage to affected areas, leading to potentially serious health complications.
Types of Amyloidosis
- AL Amyloidosis (Light Chain Amyloidosis)
- The most common form, caused by the overproduction of abnormal light chain proteins by plasma cells in the bone marrow.
- Affects organs such as the heart, kidneys, liver, and nerves.
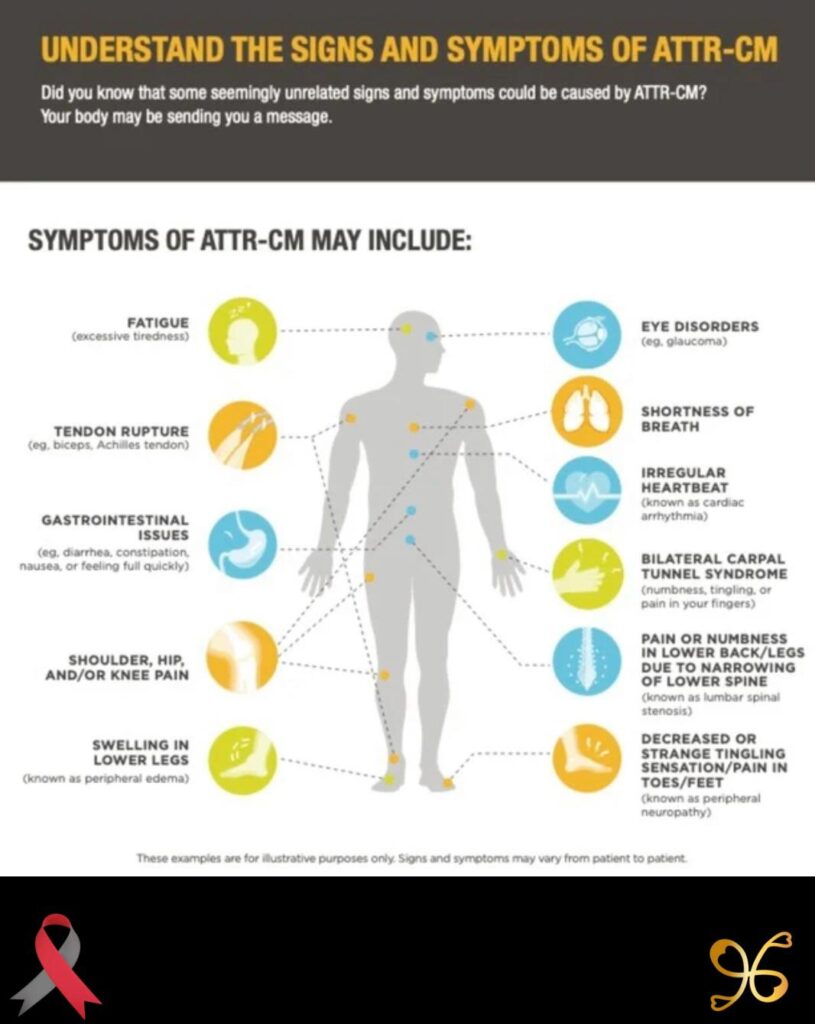
- ATTR Amyloidosis (Transthyretin Amyloidosis)
- Caused by mutations in the transthyretin (TTR) gene or by age-related changes to the protein.
- Subtypes:
- Hereditary ATTR Amyloidosis: A genetic condition affecting the nerves and heart.
- Wild-Type ATTR Amyloidosis: Typically affects older adults, primarily impacting the heart.
- AA Amyloidosis
- Results from chronic inflammatory or infectious diseases, such as rheumatoid arthritis or tuberculosis.
- Often affects the kidneys.
- Localized Amyloidosis
- Amyloid deposits occur in a single area of the body, such as the skin or bladder, rather than throughout the body.
- Other Rare Types
- Includes forms like Beta-2 Microglobulin Amyloidosis, often associated with dialysis.
Symptoms
Symptoms depend on the organs affected and may include:
- Fatigue or weakness.
- Shortness of breath.
- Swelling in the ankles or legs.
- Unintended weight loss.
- Tingling or numbness in the hands or feet.
- Enlarged tongue or difficulty swallowing (in some cases).
- Irregular heartbeat or heart failure (if the heart is affected).
- Kidney failure or protein in the urine.
Diagnosis
- Blood and Urine Tests: Detect abnormal proteins.
- Biopsy: A tissue sample confirms amyloid deposits.
- Imaging Tests: Evaluate organ damage (e.g., echocardiogram, MRI).
- Genetic Testing: Identifies hereditary forms of amyloidosis.
Treatment
Treatment focuses on managing symptoms, slowing disease progression, and addressing the underlying cause:
- Medications: Target amyloid deposits or reduce protein production (e.g., tafamidis for ATTR amyloidosis, chemotherapy for AL amyloidosis).
- Organ Transplants: For severe cases affecting organs like the heart or liver.
- Supportive Care: Treats complications such as heart failure or kidney issues.
Relevance to the Black Community
- Awareness and Access to Care: Like many rare diseases, amyloidosis may go underdiagnosed in underserved communities due to lack of awareness or healthcare access.
- Genetic Predispositions: Some hereditary forms, like ATTR amyloidosis, may disproportionately affect individuals of African descent.
Early detection and a multidisciplinary approach to treatment are essential to managing amyloidosis effectively. Collaboration with specialists and access to resources can improve outcomes and quality of life for those affected
Parkinson’s Disease is a progressive neurological disorder that affects movement, coordination, and various non-motor functions. It results from the loss of dopamine-producing neurons in a region of the brain called the substantia nigra, leading to the characteristic symptoms of the disease.
Symptoms
Parkinson’s Disease has a wide range of motor and non-motor symptoms:
Motor Symptoms
- Tremors: Shaking, typically starting in the hands or fingers, even at rest.
- Bradykinesia: Slowness of movement, making simple tasks time-consuming.
- Rigidity: Stiff muscles that may cause pain or limit range of motion.
- Postural Instability: Problems with balance and coordination, leading to a higher risk of falls.
Non-Motor Symptoms
- Cognitive changes, including memory issues or difficulty concentrating.
- Depression and anxiety.
- Sleep disturbances, such as insomnia or REM sleep behavior disorder.
- Fatigue.
- Constipation and other gastrointestinal issues.
- Loss of sense of smell (anosmia).
Causes
The exact cause of Parkinson’s is unknown, but several factors contribute to its development:
- Genetics: Mutations in certain genes (e.g., LRRK2, PARK7) can increase risk, though hereditary cases are rare.
- Environmental Factors: Exposure to toxins such as pesticides or heavy metals.
- Age: Risk increases significantly with age, typically affecting people over 60.
- Gender: Men are slightly more likely to develop Parkinson’s than women.
Diagnosis
Parkinson’s is diagnosed clinically, as no definitive lab test exists:
- Neurological Exam: Focused on motor function and reflexes.
- Imaging Tests: MRI or PET scans rule out other conditions.
- Response to Medication: Improvement with dopamine-replacement therapy supports diagnosis.
Treatment
While there is no cure, treatment focuses on managing symptoms and improving quality of life:
- Medications:
- Levodopa: Converts to dopamine in the brain to alleviate motor symptoms.
- Dopamine Agonists: Mimic dopamine’s effects.
- MAO-B Inhibitors: Slow the breakdown of dopamine.
- Surgical Options:
- Deep Brain Stimulation (DBS): Implants electrodes in the brain to regulate abnormal activity.
- Lifestyle and Supportive Therapies:
- Physical, occupational, and speech therapy.
- Regular exercise to improve mobility and balance.
- Dietary adjustments to manage constipation and maintain energy levels.
- Mental Health Support:
- Counseling for anxiety or depression.
- Support groups for patients and families.
Parkinson’s in the Black Community
- Underdiagnosis and Delayed Treatment: Parkinson’s may be underrecognized in Black patients due to healthcare disparities or biases.
- Awareness and Access: Outreach and education are critical for improving early diagnosis and care in underserved communities.
- Research Gaps: Increased representation in clinical studies is needed to understand disease progression and outcomes in Black populations.
Living with Parkinson’s
Parkinson’s requires a multidisciplinary approach, involving neurologists, therapists, and caregivers. With proper management, many patients maintain independence and lead fulfilling lives for many years after diagnosis. Early intervention and a supportive network are key to improving quality of life.
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system—that’s the brain, spinal cord, and optic nerves. In MS, the body’s immune system attacks the protective coating (myelin) that surrounds nerve fibers. This causes communication problems between the brain and the rest of the body.
Over time, it can cause nerve damage and disability.
Common Symptoms of MS
MS symptoms vary from person to person, and they can come and go (relapse) or steadily worsen over time. Common symptoms include:
Symptom | Description |
Numbness or tingling | Often in the face, arms, or legs |
Muscle weakness or spasms | Trouble walking or holding things |
Vision problems | Blurry or double vision, sometimes partial loss |
Fatigue | Extreme tiredness, even after rest |
Dizziness or balance issues | Feeling off-balance or lightheaded |
Memory or focus issues | “Brain fog,” forgetfulness |
Slurred speech | Trouble speaking clearly |
Bladder or bowel issues | Urgency or difficulty |
What Causes MS?
The exact cause is unknown, but it’s believed to be a mix of:
- Genetics
- Environmental triggers
- Immune system malfunction
Types of MS
- Relapsing-Remitting MS (RRMS)
Most common (about 85%). Flare-ups followed by periods of recovery. - Secondary Progressive MS (SPMS)
Starts as RRMS, then gradually worsens. - Primary Progressive MS (PPMS)
Steady worsening from the start, with no clear relapses or remissions. - Progressive-Relapsing MS (PRMS)
Rare; steady worsening with occasional relapses.
How is MS Diagnosed?
- MRI scans (to see brain/spinal cord damage)
- Spinal tap (lumbar puncture)
- Blood tests
- Neurological exams
Is There a Cure?
No cure yet, but treatments can slow the disease, reduce relapses, and manage symptoms, such as:
- Disease-modifying therapies (DMTs)
- Physical therapy
- Medications for fatigue, pain, or muscle stiffness
- Lifestyle changes: healthy eating, rest, stress reduction
MS & the Black Community
- MS was once thought to be rare in Black individuals, but new research shows it’s often underdiagnosed.
- Black people may experience more aggressive symptoms and faster progression, especially with mobility and vision.
- Early diagnosis and care are crucial to slowing progression and protecting quality of life.
Lupus can impact:
- Skin
- Joints
- Kidneys
- Heart
- Lungs
- Brain
- Blood cells
Common Symptoms
Lupus symptoms vary but may include:
Symptom | Description |
Fatigue | Extreme tiredness, even after resting |
Joint pain & swelling | Especially in hands, wrists, and knees |
Skin rashes | Often a “butterfly” rash across the cheeks/nose |
Sun sensitivity | Rashes or flares triggered by sunlight |
Hair loss | Due to inflammation |
Kidney issues | Swelling in legs, weight gain, foamy urine |
Chest pain | Especially when taking deep breaths |
Brain fog or memory issues | Trouble concentrating |
Types of Lupus
- Systemic Lupus Erythematosus (SLE)
The most common and serious type—can affect multiple organs. - Cutaneous Lupus
Affects the skin; includes rashes and lesions. - Drug-Induced Lupus
Caused by certain medications and often goes away when the drug is stopped. - Neonatal Lupus
Rare; affects infants born to mothers with lupus-related antibodies.
Diagnosis
There’s no single test. Doctors use:
- Blood tests (like ANA)
- Urine tests
- Physical exams
- Imaging (if organs are affected)
It can take time to diagnose because symptoms can mimic other illnesses.
Treatment
There’s no cure, but lupus can be managed. Treatments may include:
- Anti-inflammatory drugs (for pain and swelling)
- Steroids (to reduce immune response)
- Immunosuppressants (to calm the immune system)
- Antimalarials (like hydroxychloroquine)
Lupus & Black Communities
- Lupus is 3 times more common in Black women than in white women.
- It often appears earlier and more severely in Black and Hispanic individuals.
- Awareness, access to care, and early diagnosis are critical.
- In ITP, the immune system mistakes platelets as a threat and destroys them.
- It may happen after a viral infection, certain medications, or sometimes with no known cause.
- It can also be linked to other autoimmune conditions, like lupus.
Who Can Get ITP?
- Children: Often after a viral infection; usually temporary.
- Adults: More common in women under 40, but can affect anyone.
How Is ITP Diagnosed?
Doctors may use:
- Blood tests (to count platelets and rule out other issues)
- Physical exams
- Sometimes a bone marrow test (in complex cases)
How Is It Treated?
Treatment depends on how low the platelet count is and how serious the bleeding is.
Options include:
- Corticosteroids (like prednisone)
- IV immunoglobulin (IVIG)
- Platelet transfusions
- Medications that boost platelet production
- In rare or severe cases, spleen removal surgery (splenectomy)
Some people with mild ITP don’t need treatment—just regular monitoring.
ITP & the Black Community
- Like other autoimmune diseases, ITP can be underdiagnosed or misdiagnosed in Black individuals due to health disparities.
- Awareness and early diagnosis are important—especially when unexplained bruising or bleeding occurs.
In Summary
ITP is a blood disorder where your immune system attacks platelets, leading to bruising, bleeding, and low clotting ability. With proper care, most people live full, healthy lives.
COLLEGE AND CAREER EXPO FAQS
GENERAL QUESTIONS
• A notebook or phone to take notes
• Questions for colleges, employers, and mentors
• An open mind and positive attitude!
PARENT & GUARDIAN QUESTIONS
• College application timelines
• FAFSA and financial aid
• Career exploration
• Preparing your student for life after graduation
COLLEGE & CAREER REP QUESTIONS
EVENT LOGISTICS
WE ARE ONE: ONE HEART, MANY SEASONS EMPOWERMENT COUPLES RETREAT
Couples Empowerment Retreat — FAQs
GENERAL INFORMATION
3030 Holiday Drive, Fort Lauderdale, FL 33316
Check-in begins at 3 pm with the welcome session starting at 6 pm.
REGISTRATION & ACCOMMODATIONS
• Welcome gift bag
• Daily breakfast & one evening dinner
• Access to resort amenities • Surprise couple experiences
COUPLE EXPERIENCE & EXPECTATIONS
• Swimwear for beach or spa time
• Journals or notebooks for reflection
• Openness to grow, laugh, and reconnect
EVENING EXPERIENCES
• Daily Empowerment Sessions: Comfortable clothing
• Date Night Dinner: Elegant & Fly – dress to impress
• Final Recommitment Vow Renewal (optional): Beach Formal (barefoot encouraged!)
OTHER IMPORTANT NOTES
Or text: 786.828.2290